Helping Advance Health Care
Clinical trials are key to advancing medicine and science. You can help by joining a trial. Here’s what you should know.
By Jill Tyrer | Sept. 14, 2022
You can make a difference in helping to find better treatments for arthritis. The Arthritis Foundation, doctors and researchers are invested in clinical trials that push us closer to life-changing therapies — and you can help by participating in a clinical trial.
Clinical trials are key to finding new ways to prevent, detect or treat diseases. By participating, you are not only helping other people who live with a chronic disease like arthritis that doesn’t yet have a cure, you might also help yourself.
Women and minorities are especially needed to participate to help promote health equity. In February 2022, Trinity Life Sciences reported that although racial and ethnic minorities comprise more than 40% of the U.S. population, only 5% to 10% of those who participate in clinical trials typically represent these groups. For example, according to the Trinity report: In 2017, of more than 59,000 participants in 46 new drug trials approved by the Center for Drug Evaluation and Research (CDER), 77% were white. More than 80% of participants in studies of the genome were of European ancestry. Pfizer reported in 2019 that nearly 81% of its clinical trial participants were white, compared with 14% African American, 16% Hispanic American and 3% Asian American.
This is true even for diseases that occur at higher rates among certain minority populations, such as diabetes.
As a result, the data and findings that come out of these studies do not adequately represent people who are not white. Individuals respond in different ways to treatments, and genetic factors also play a role in how people respond.
“For example, variations in genetic coding can make a treatment more or less toxic for one racial or ethnic group than another. These variations can also make drugs like antidepressants and blood-pressure medications less effective for certain groups,” according to the Food and Drug Administration, which has issued guidance to increase diversity in clinical trials. Participants in clinical trials should represent those who are likely to take the drug or treatment being tested.
Obstacles to participation by non-whites include mistrust due to past abuses, language barriers, lack of transportation, competing responsibilities, and lack of communication and information. To ensure that all Americans receive adequate and equitable health care, however, it’s especially important for non-white Americans to participate in trials.
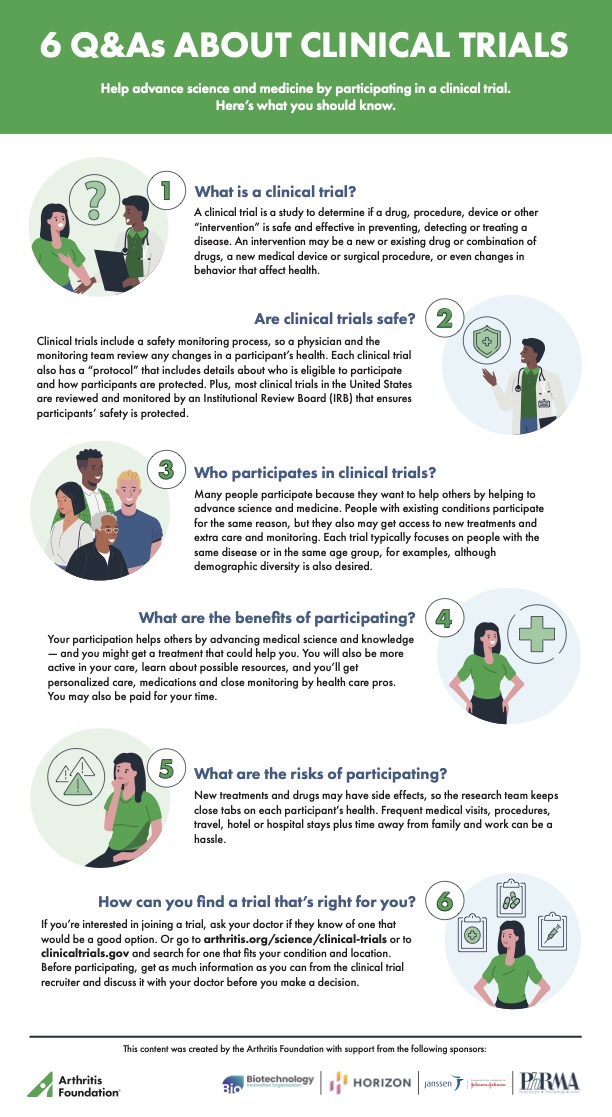
Click the image below to download the pdf file 6 Q&As About Clinical Trials
Here’s what you should know about clinical trials.
You can make a difference in helping to find better treatments for arthritis. The Arthritis Foundation, doctors and researchers are invested in clinical trials that push us closer to life-changing therapies — and you can help by participating in a clinical trial.
Clinical trials are key to finding new ways to prevent, detect or treat diseases. By participating, you are not only helping other people who live with a chronic disease like arthritis that doesn’t yet have a cure, you might also help yourself.
Women and minorities are especially needed to participate to help promote health equity. In February 2022, Trinity Life Sciences reported that although racial and ethnic minorities comprise more than 40% of the U.S. population, only 5% to 10% of those who participate in clinical trials typically represent these groups. For example, according to the Trinity report: In 2017, of more than 59,000 participants in 46 new drug trials approved by the Center for Drug Evaluation and Research (CDER), 77% were white. More than 80% of participants in studies of the genome were of European ancestry. Pfizer reported in 2019 that nearly 81% of its clinical trial participants were white, compared with 14% African American, 16% Hispanic American and 3% Asian American.
This is true even for diseases that occur at higher rates among certain minority populations, such as diabetes.
As a result, the data and findings that come out of these studies do not adequately represent people who are not white. Individuals respond in different ways to treatments, and genetic factors also play a role in how people respond.
“For example, variations in genetic coding can make a treatment more or less toxic for one racial or ethnic group than another. These variations can also make drugs like antidepressants and blood-pressure medications less effective for certain groups,” according to the Food and Drug Administration, which has issued guidance to increase diversity in clinical trials. Participants in clinical trials should represent those who are likely to take the drug or treatment being tested.
Obstacles to participation by non-whites include mistrust due to past abuses, language barriers, lack of transportation, competing responsibilities, and lack of communication and information. To ensure that all Americans receive adequate and equitable health care, however, it’s especially important for non-white Americans to participate in trials.
Click the image below to download the pdf file 6 Q&As About Clinical Trials
Here’s what you should know about clinical trials.
- What is a clinical trial?
- Are clinical trials safe?
- Who participates in clinical trials?
- What are the benefits of participating?
- Helping others by advancing medical science and knowledge.
- Potentially getting a treatment that might help you.
- Being more active in your care and learning about other possible resources.
- Receiving personalized care, including physician exams, nurse evaluations, laboratory studies and medications.
- Monetary compensation for participants’ time.
- What are the risks of participating?
- Members of the research team monitor each participant’s health, but there are potential side effects from new treatments or medications.
- Potential hassles and inconvenience of frequent medical visits, tests and procedures, travel, hotel or hospital stays and time away from family, work and routine.
- You may not receive the treatment; instead, you might be in the “control” group that receives standard treatment or placebo.
- How can you find a trial that's right for you?
Questions to Ask Before Joining a Clinical Trial
Before signing up for a clinical trial, get the information you need from the research team. Ask a friend or family member to join you to learn more, take notes and record the discussion. Start with these questions, and don’t hesitate to add your own:- What is the goal of the study?
- Why do the researchers believe it’s a good idea?
- Will I know what intervention I receive?
- Is there an IRB?
- What will I need to do and what will be expected of me?
- What measures are in place to protect my safety?
- What recourse will I have if I am injured?
- How will this affect my existing arthritis treatment?
- Will it involve travel, hospital stays, time off work or time away from my family?
- Will it cost me any money to participate?
- If so, how much?
- Will my insurance cover any potential costs?
- Will I be financially compensated for my time?
- Will I be reimbursed for travel or other expenses?
- What measures are being taken to protect my privacy?
- How might participating benefit me?
- What potential risks would I have?
- How long will it last?
- How will I find out about the study results?
- If the treatment helps me, will I be able to continue it?
- What long-term effects and follow-up can I expect?